Ghana
Digital Health and Inequality: Technology’s Role in Ghana’s fight against Diabetes and Hypertension
- Status
- Completed Research
- Research Year
- 2024-25
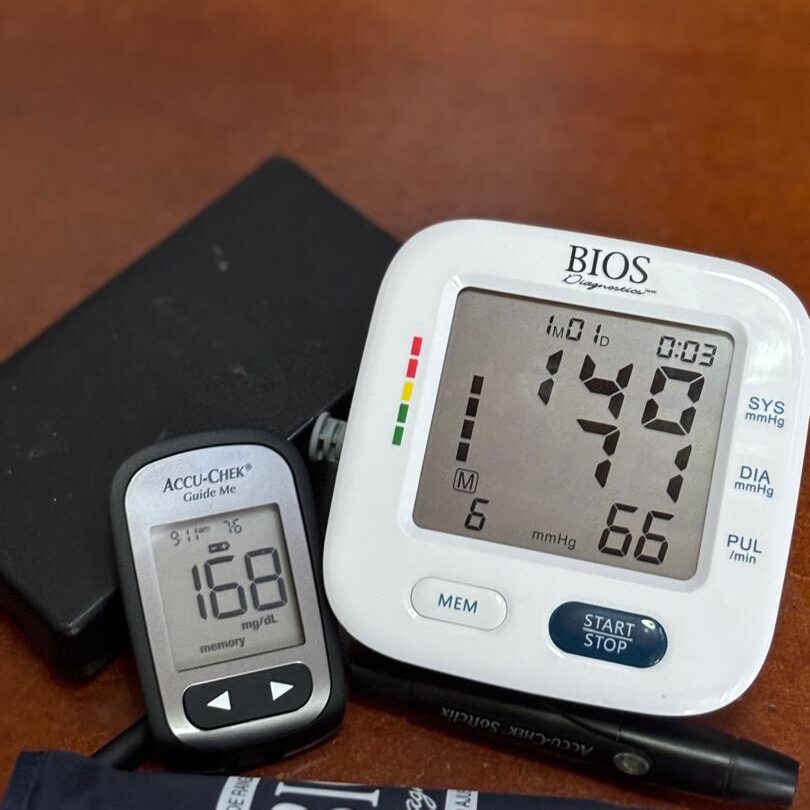
Ghana faces a significant health challenge as it grapples with the dual burden of communicable and non-communicable diseases (NCDs). According to the World Health Organization (2023), NCDs account for approximately 41 million deaths globally, with low- and middle-income countries bearing the brunt. As a middle-income country, Ghana experiences 43% of all-cause mortality due to NCDs, particularly cardiovascular diseases (CVDs) and diabetes mellitus (DM), which represent the most pressing NCD-related health concerns in the nation. The critical connection between poorly managed diabetes and increased cardiovascular risks highlights the urgent need for effective interventions to address these interlinked health issues. Technological advancements, such as continuous glucose monitors, insulin pumps, and telehealth services, have emerged as vital tools in the global effort to manage diabetes and prevent CVDs. However, the adoption of these innovative technologies remains limited in Ghana, especially in hard-to-reach communities where access to healthcare resources is limited.
This project aims to evaluate the health technologies available for managing DM and CVD while investigating the barriers that hinder their implementation in underserved areas. The team will explore key questions regarding the level of awareness among healthcare providers and patients, the obstacles to technology adoption, the feasibility of use in these communities, and practical solutions for integrating these technologies effectively.
Researchers
Mentors
-

-

-

Ashesi University
Disraeli Asante-Darko
Head of Business Administration Department, Ashesi University