Rwanda
Expanded Program on Immunization: Near-universal Childhood Vaccination Rates
- Status
- Completed Research
- Research Year
- 2016-17
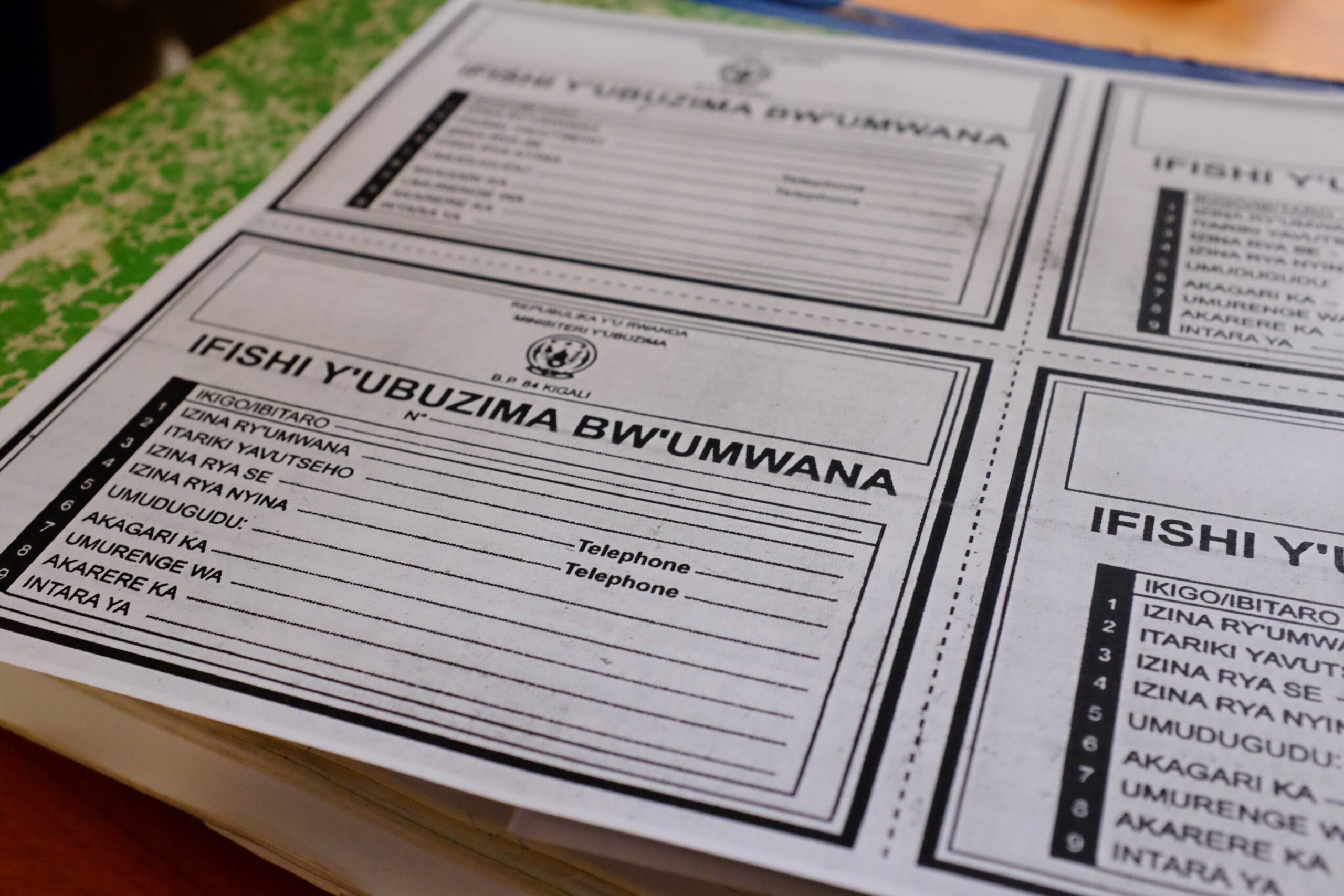
Geography, a large rural population and extreme poverty, compounded with the 1994 genocide, all contributed to the challenges facing widespread childhood vaccinations. Rwanda scaled up its immunization program and other health and development programs to meet the Millennium Development Goals. Despite its geographic and historic barriers to improving child mortality outcomes, its immunization program clearly demonstrates effective reach.
Researchers
-

-

-
-

University of Toronto
Julia Robson
Mentors
-

University of Toronto
Stanley Zlotkin
Professor of Paediatrics, Public Health Sciences and Nutritional Sciences at the Hospital for Sick Children and University of Toronto; Chief at the Centre for Global Child Health, The Hospital for Sick Children
Related Information
-

International Journal of Healthcare
Making sense of Rwanda’s remarkable vaccine coverage success
-

-

The Lancet
Near universal childhood vaccination rates in Rwanda: how was this achieved and can it be duplicated?

