Mozambique
Public-Private Partnerships for Global Health: The mVacciNation Pilot in Mozambique
- Status
- Completed Research
- Research Year
- 2020-21
Vaccination coverage for several routine vaccines is less than 75 per cent in many parts of in Mozambique, and the under-five mortality rate remains high at 97 deaths per 1,000 live births. A cross sector partnership established the mVacciNation (mVacc) program in 2014 to help tackle the issue of low vaccination coverage among children under the age of five. mVacc is a program based on the use of a mobile phone application. The application is used by healthcare workers to capture and record the vaccinations and health records of each child. With this data, they forecast and optimize vaccine stock levels and follow up with each child’s caregiver via SMS to remind them of upcoming vaccination appointments. Healthcare workers and program managers are able to track vaccine stock levels and ensure safe storage by immediately addressing any issues in the cold chain. The data is then synced and centrally stored on the Ministry of Health cloud, enabling the app to be integrated into existing data management systems.
Researchers
-

-

University of Toronto
Muhammad Sajid
-

-

-
Mentors
-

University of Toronto
Erica Di Ruggiero
Associate Professor of Global Health and Director of the Centre for Global Health, Dalla Lana School of Public Health, University of Toronto
Related Information
-
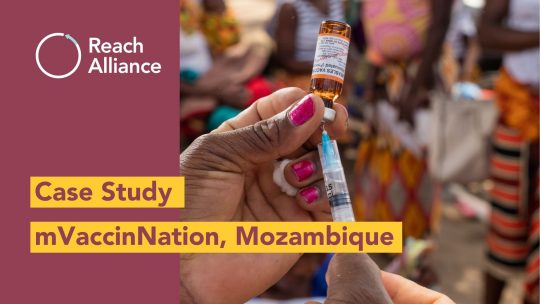
How mVaccinNation tackled low vaccination coverage in Mozambique