In 1988, India had an estimated 200,000 polio cases per year and was one of the last countries to track and report cases of polio. Since then, the country consistently improved its polio vaccination and preventative healthcare programs. The polio program’s success can be attributed to motivated central leadership combined with comprehensive local commitment. By 2014, the WHO declared India to be polio-free.
Researchers
Mentors
-

University of Toronto
Anita McGahan
University Professor and George E. Connell Chair in Organizations and Society, Rotman School of Management; Professor, Munk School of Global Affairs & Public Policy, University of Toronto
Related Information
-

BMJ Global Health
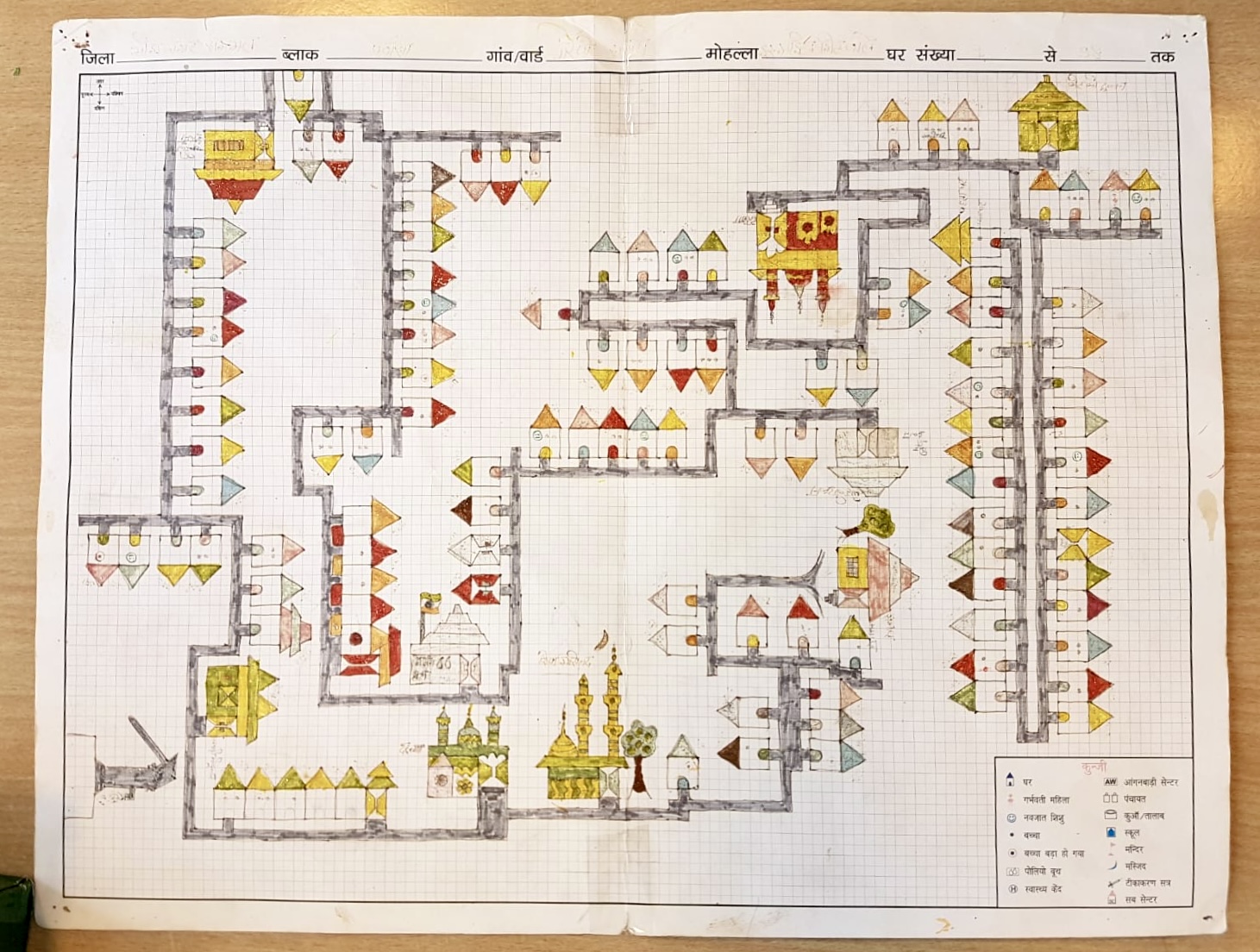
Overcoming vaccine deployment challenges among the hardest to reach: lessons from polio elimination in India
-

Media
To overcome vaccine hesitancy, governments need to show citizens what’s in it for them




